The Conversation Project in the Fredericksburg Region
- Category: Community Resources
- Posted On:

What is The Conversation Project?
The Conversation Project is a movement to help remind people, regardless of age or current health, of the importance of having end of life conversations with friends and loved ones before end of life.
It is a movement to help encourage all of us to continue to learn about protecting and honoring our wishes for future medical care.
Why It Is Important?
90% of people say that talking with their loved ones about end of life care is important, yet 27% have actually done so.
70% of people say they prefer to die at home, yet 70% die in a hospital, nursing home, or long-term care facility.
80% of people say that if seriously ill they would want to talk to their doctor about end of life care, yet 7% report having had an end of life conversation with their doctor.
How The Conversation Project Started
In 2010 after the death of her mother, Ellen Goodman and a group of colleagues and concerned media, clergy, and medical professionals gathered to share stories of “good deaths” and “bad deaths” within their own circle of loved ones.
In 2011, the group collaborated with the Institute for Healthcare Improvement (IHI). Together they developed The Conversation Project.
A Century of Change
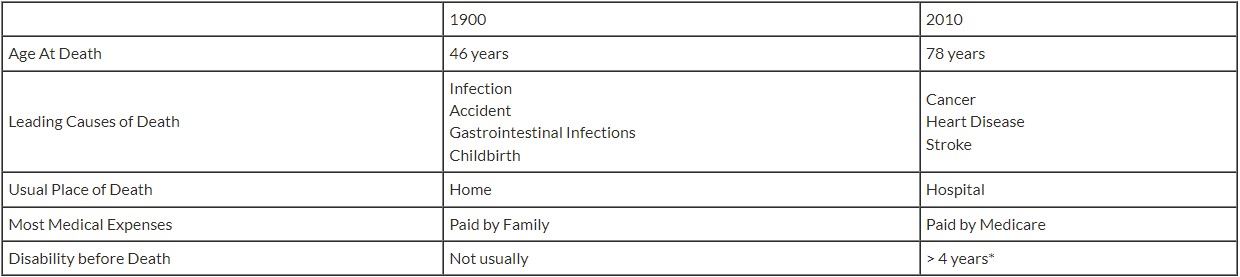
*Joanne Lynn, MD 2001
Why don’t we want to talk about end of life?
- Belief that modern medical care can do anything
- Fear that talking about it might tempt fate (superstitions)
- Talking about it is hard for us and can bring up tender and strong emotions
- The conversation may upset someone – it reminds us of our vulnerability
- Reluctant to discuss terminal condition
- We may be perceived by family and/or physician as “giving up”
- We are confused by false choices (choosing to die or not)
What a conversation can do is provide a shared understanding of what matters most to you and your loved ones. Having the conversation can help make it easier to make decisions when the time comes.
Step 1: Get Ready
You don’t need to talk about it just yet. Just think about it.
You can start out by writing a letter – to yourself, a loved one, or a friend.
Step 2: Get Set
Write down a what-matters-to-you-most statement. How do you want to live?
Think about what you want for end-of-life care. What do you value most? What can you not imagine living without?
- How long do you want to receive medical care?
- How involved do you want your loved ones to be?
- What role do you want your loved ones to play?
Step 3: Go!
When you are ready to have the conversation, start with the basics.
Who do you want to talk to? Who do you trust to speak for you?
When would be a good time to talk?
Where would you feel comfortable talking?
What do you want to be sure to say?
Step 4: Keep Going
Now that you have had the conversation, write it down and keep having the conversation.
Advance Care Planning: the process of thinking about your wishes
Advance Directive: a document that describes your wishes
Health Care Proxy: identifies your health care agent, (often called your proxy) the person you trust to act on your behalf if you are unable to make health care decisions or communicate your wishes (also called Durable Power of Attorney for Health Care)
Living Will: a written statement detailing a person's desires regarding their medical treatment in circumstances in which they are no longer able to express informed consent
What is an Advance Directive?
An Advance Directive is a free legal document that describes your wishes.
It tells healthcare providers:
- Who you assign to make medical decisions for you if you are unable to make those decisions. (Medical POA)
- What treatments you want or do not want at end of life. (Living Will)
Another Option for an Advance Directive: The Five Wishes
The Five Wishes is a living will that talks about your personal, emotional and spiritual needs as well as your medical wishes.
Documents the answers to five questions:
- Who is the person(s) I want to make care decisions for me if I cannot?
- What kind of medical treatment I want or don’t want?
- How comfortable do I want to be?
- How do I want people to treat me?
- What do I want my loved ones to know?

.jpg)

